Leads on ECG: 12 Essential Facts You Must Know Now
Ever wondered how a simple ECG can reveal the secrets of your heart? It all starts with understanding the leads on ECG—your heart’s electrical storytellers.
What Are Leads on ECG and Why They Matter

The term leads on ECG refers to the specific views or angles from which the heart’s electrical activity is recorded. These leads are not physical locations on the heart but rather mathematical representations of voltage differences between electrodes placed on the skin. Understanding these leads is crucial for accurate diagnosis of cardiac conditions such as arrhythmias, myocardial infarctions, and conduction abnormalities.
Definition of ECG Leads
An electrocardiogram (ECG or EKG) records the electrical impulses generated by the heart during each cardiac cycle. The leads on ecg are essentially the pathways through which these electrical signals are measured. Each lead provides a unique perspective of the heart’s electrical activity, allowing clinicians to assess different regions of the myocardium.
- There are 12 standard leads in a conventional ECG: 6 limb leads and 6 precordial (chest) leads.
- Each lead measures the voltage difference between two or more electrodes.
- Leads are labeled based on their anatomical orientation (e.g., Lead I, II, III, aVR, aVL, aVF, V1–V6).
How ECG Leads Capture Heart Activity
The heart generates electrical impulses that spread through the myocardium, causing depolarization and repolarization of cardiac cells. These electrical changes create small voltages that can be detected on the body surface. The leads on ecg act as sensors, translating these microvolt-level signals into waveforms displayed on the ECG paper or digital monitor.
For example, Lead I measures the electrical potential between the right and left arms, providing a horizontal view of the heart’s activity. This allows clinicians to detect left-to-right axis deviations or lateral wall ischemia.
“The 12-lead ECG is one of the most powerful diagnostic tools in cardiology—when interpreted correctly.” — Dr. Eric Topol, Scripps Research
The 12 Standard Leads on ECG Explained
A standard 12-lead ECG provides a comprehensive snapshot of the heart’s electrical function from multiple angles. These 12 leads are divided into two main groups: the limb leads and the precordial leads. Each group plays a distinct role in evaluating cardiac health.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Limb Leads: The Frontal Plane Perspective
The limb leads consist of six leads that view the heart in the frontal plane. They include three bipolar limb leads (I, II, III) and three augmented unipolar limb leads (aVR, aVL, aVF).
- Lead I: Measures voltage between the right and left arms.
- Lead II: Between right arm and left leg—often used for rhythm monitoring.
- Lead III: Between left arm and left leg.
- aVR: Looks at the heart from the right shoulder; often reciprocal to other leads.
- aVL: Views the lateral wall of the left ventricle.
- aVF: Assesses inferior wall activity.
These leads help determine the heart’s electrical axis, identify inferior or lateral myocardial infarctions, and detect limb lead reversals.
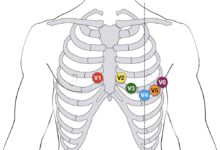
Precordial Leads: The Horizontal Plane Insight
The six precordial (chest) leads—V1 through V6—are placed across the chest wall and provide a horizontal plane view of the heart. They are essential for detecting anterior, septal, and lateral wall abnormalities.
- V1 and V2: Over the right ventricle and interventricular septum—ideal for detecting septal infarcts.
- V3 and V4: Over the anterior wall of the left ventricle.
- V5 and V6: Over the lateral wall—useful for diagnosing lateral MI.
Proper placement is critical. Misplacement of V1 or V2 can lead to misdiagnosis of right bundle branch block or anterior MI. For accurate results, V1 is placed in the 4th intercostal space at the right sternal border, while V2 is at the left sternal border.
How Leads on ECG Represent Different Heart Regions
Each of the leads on ecg corresponds to a specific anatomical region of the heart. This regional correlation allows clinicians to localize cardiac pathology with remarkable precision.
Anterior Wall: Leads V1–V4
The anterior wall of the heart is primarily viewed through leads V1 to V4. These leads are particularly sensitive to changes associated with anterior myocardial infarction.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
- ST elevation in V1–V4 suggests anterior wall STEMI (ST-elevation myocardial infarction).
- Pathological Q waves in these leads indicate prior infarction.
- V1 is especially useful in diagnosing right bundle branch block (RBBB) due to its proximity to the septum.
For example, occlusion of the left anterior descending (LAD) artery typically manifests as ST elevation in V1–V4. This is why the LAD is often called the “widowmaker” artery.
Inferior Wall: Leads II, III, aVF
The inferior wall of the heart is best visualized using the inferior leads: II, III, and aVF. These limb leads detect electrical activity moving downward toward the diaphragm.
- ST elevation in II, III, aVF indicates inferior MI, often due to right coronary artery (RCA) occlusion.
- Reciprocal ST depression may appear in aVL and I.
- Right ventricular infarction can be assessed by adding right-sided leads (V4R).
It’s important to note that Lead III can sometimes show more pronounced ST elevation than II or aVF in inferior MI, but clinicians must rule out lead misplacement before making a diagnosis.
Understanding Bipolar vs. Unipolar Leads
One of the foundational concepts in ECG interpretation is distinguishing between bipolar and unipolar leads. Both types contribute to the 12-lead system but function differently in capturing electrical activity.
Bipolar Limb Leads (I, II, III)
Developed by Willem Einthoven, the father of modern electrocardiography, the bipolar limb leads measure the voltage difference between two limbs.
- Lead I: Right arm (–) to left arm (+)
- Lead II: Right arm (–) to left leg (+)
- Lead III: Left arm (–) to left leg (+)
These leads form what is known as Einthoven’s Triangle. According to StatPearls, this triangular configuration allows for the calculation of the heart’s electrical axis in the frontal plane.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Augmented Unipolar Limb Leads (aVR, aVL, aVF)
Unlike bipolar leads, the augmented leads are unipolar, meaning they measure the voltage at one electrode relative to a central reference point (Wilson’s central terminal).
- aVR: Measures activity toward the right shoulder.
- aVL: Toward the left shoulder.
- aVF: Toward the left foot.
Because aVR looks at the heart from the opposite direction of most other leads, it often shows inverted P waves, QRS complexes, and T waves. However, significant ST elevation in aVR can indicate severe global ischemia or left main coronary artery disease.
“ST elevation in aVR with diffuse ST depression elsewhere is a red flag for left main or triple-vessel disease.” — UpToDate, Cardiology Section
The Role of Precordial Leads in Diagnosing Myocardial Infarction
The precordial leads (V1–V6) are indispensable in diagnosing myocardial infarction, especially when it involves the anterior or lateral walls of the left ventricle.
Anterior Myocardial Infarction and Leads V1–V4
Anterior MI is one of the most dangerous types due to the large amount of myocardium affected. It is typically caused by occlusion of the left anterior descending (LAD) artery.
- ST elevation in V1–V4 is the hallmark ECG finding.
- New left bundle branch block (LBBB) with clinical symptoms also suggests anterior STEMI.
- Reciprocal changes may be seen in inferior leads (II, III, aVF).
Early recognition via leads on ecg can save lives. According to the American Heart Association, door-to-balloon time should be under 90 minutes for optimal outcomes in STEMI patients.
Lateral Myocardial Infarction and Leads I, aVL, V5–V6
Lateral wall MI is less common but still significant. It is usually due to occlusion of the left circumflex artery (LCx) or a diagonal branch of the LAD.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
- ST elevation in I, aVL, V5, and V6 indicates lateral involvement.
- Reciprocal ST depression may appear in V1–V3.
- aVL is particularly useful for detecting high lateral wall infarcts.
Because lateral MI can be subtle, clinicians must pay close attention to voltage changes and T-wave inversions in these leads.
Common Misinterpretations of Leads on ECG
Even experienced clinicians can misinterpret ECG findings if they misunderstand the function and orientation of the leads on ecg. Misdiagnosis can lead to inappropriate treatment or missed emergencies.
Lead Reversal: A Frequent Pitfall
Arm lead reversal (right and left arm electrodes swapped) is one of the most common technical errors. It can mimic dextrocardia or MI patterns.
- Lead I shows inverted P waves, QRS complexes, and T waves.
- Lead aVR may appear upright instead of negative.
- Lead II and III get swapped, altering axis interpretation.
Clues to detect reversal include normal R-wave progression in precordial leads despite apparent dextrocardia and positive P waves in aVL.
Incorrect Chest Lead Placement
Placing V1 and V2 too high or too lateral can distort readings. For instance, high placement may mimic anterior MI or right ventricular hypertrophy.
- V1 misplaced in the 2nd or 3rd intercostal space can exaggerate R waves, mimicking posterior MI.
- Failure to place V4R when suspecting right ventricular infarction can delay treatment.
- Rotating the patient or using anatomical landmarks improves accuracy.
A study published in European Heart Journal – Cardiovascular Imaging found that up to 40% of ECGs have some degree of lead misplacement, emphasizing the need for standardized protocols.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Advanced Applications of Leads on ECG
Beyond the standard 12-lead ECG, advanced applications use modified lead configurations to detect hidden pathologies or improve diagnostic yield.
Right-Sided ECG (V4R)
When inferior MI is present, right-sided leads—especially V4R—can detect right ventricular infarction.
- V4R is placed in the 5th intercostal space at the midclavicular line on the right side.
- ST elevation ≥1 mm in V4R is highly specific for right ventricular infarction.
- RV infarction increases the risk of hemodynamic instability and requires cautious fluid management.
According to the 2020 AHA Guidelines, V4R should be considered in all patients with inferior STEMI.
Posterior Leads (V7–V9)
Posterior MI is often missed because standard leads don’t directly view the posterior wall. However, posterior leads (V7–V9) placed on the back can reveal ST elevation in this region.
- V7: Left posterior axillary line.
- V8: Left scapular line.
- V9: Left paraspinal area.
Alternatively, clinicians can suspect posterior MI if there is ST depression and tall R waves in V1–V2 (mirror image changes). Early detection prevents complications like ventricular rupture.
Interpreting ECG Axis Using Leads on ECG
The electrical axis of the heart reflects the overall direction of ventricular depolarization. It is determined primarily by analyzing the QRS complex in the limb leads.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Normal vs. Abnormal Axis Deviation
The normal QRS axis ranges from -30° to +90°. Deviations outside this range suggest underlying pathology.
- Left Axis Deviation (-30° to -90°): Seen in left anterior fascicular block, inferior MI, or left ventricular hypertrophy.
- Right Axis Deviation (+90° to +180°): Associated with right ventricular hypertrophy, pulmonary embolism, or chronic lung disease.
- Extreme Axis Deviation (-90° to -180°): Rare; may indicate ventricular tachycardia or lead reversal.
Quick method: If QRS is positive in I and aVF, axis is normal. If positive in I but negative in aVF, it’s left axis. If negative in I and positive in aVF, it’s right axis.
Using Leads I and aVF to Determine Axis
Leads I and aVF are perpendicular to each other, forming a coordinate system for axis determination.
- Lead I represents the horizontal axis (left = positive, right = negative).
- aVF represents the vertical axis (inferior = positive, superior = negative).
- By combining the deflection in both leads, you can estimate the quadrant of the axis.
For example, a tall R wave in aVF and small QRS in I suggests right axis deviation, possibly due to cor pulmonale.
Practical Tips for Accurate ECG Lead Placement
Even the most advanced ECG machine cannot compensate for poor electrode placement. Accuracy begins with proper technique and attention to detail.
Step-by-Step Guide to Limb Lead Placement
Limb leads should be placed on the fleshy parts of the limbs, not over bony prominences or joints.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
- Right arm electrode: Inner aspect of the right forearm.
- Left arm electrode: Inner aspect of the left forearm.
- Left leg electrode: Inner aspect of the left lower leg.
- Right leg electrode: Ground; usually on the right lower leg.
Ensure skin is clean and dry. Use alcohol wipes if necessary. Avoid placing electrodes over areas with muscle tremor or electrical interference.
Correct Precordial Lead Positioning
Precordial leads must follow precise anatomical landmarks.
- Locate the 4th intercostal space at the right sternal border for V1.
- Same level on the left sternal border for V2.
- V3 is midway between V2 and V4.
- V4: 5th intercostal space at the midclavicular line.
- V5: Same horizontal level as V4, at the anterior axillary line.
- V6: Midaxillary line, same level as V4.
In women, place V3–V6 on the chest wall, not on breast tissue, to avoid signal attenuation.
“Proper lead placement is the foundation of an interpretable ECG.” — Life in the Fast Lane Medical Education
FAQs About Leads on ECG
What are the 12 leads on an ECG?
The 12 leads on an ECG consist of six limb leads (I, II, III, aVR, aVL, aVF) and six precordial leads (V1–V6). Together, they provide a 3D view of the heart’s electrical activity, allowing for precise localization of cardiac abnormalities.
Why is lead V1 important in ECG interpretation?
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Lead V1 is crucial because it sits over the interventricular septum and right ventricle. It helps diagnose right bundle branch block, posterior MI (via mirror changes), and arrhythmias like atrial fibrillation. Its position makes it sensitive to septal and right-sided heart issues.
Can lead placement affect ECG results?
Yes, incorrect lead placement can significantly alter ECG readings. For example, misplaced V1 can mimic anterior MI, and arm lead reversal can simulate dextrocardia. Proper training and adherence to anatomical landmarks are essential for accurate diagnosis.
What does ST elevation in lead aVR mean?
ST elevation in lead aVR, especially when accompanied by widespread ST depression, may indicate severe global ischemia, left main coronary artery occlusion, or multivessel disease. It’s a critical finding requiring immediate intervention.
How do you identify inferior myocardial infarction on ECG?
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Inferior MI is identified by ST elevation in leads II, III, and aVF. Reciprocal ST depression may appear in leads I and aVL. It’s often caused by occlusion of the right coronary artery and may be associated with right ventricular infarction.
Understanding the leads on ecg is fundamental to mastering ECG interpretation. From diagnosing life-threatening infarctions to detecting subtle conduction delays, each lead tells a story. By mastering their placement, orientation, and clinical significance, healthcare providers can unlock the full diagnostic power of the 12-lead ECG. Whether you’re a medical student, nurse, or physician, a deep understanding of these leads enhances patient care and improves outcomes.
Further Reading: